Panniculectomy covered by insurance aetna is a significant factor for individuals considering this procedure. This guide provides a comprehensive overview, exploring the procedure, Aetna’s coverage policies, pre-operative considerations, and the claim process. Understanding your options is key to making informed decisions about your health and well-being.
This in-depth analysis will walk you through the various aspects of a panniculectomy, focusing on Aetna’s specific coverage criteria, and the steps involved in navigating the insurance claim process. We’ll also compare panniculectomy to alternative body contouring procedures, discussing potential complications and recovery timelines. Ultimately, this resource aims to empower you with the knowledge needed to confidently approach this procedure.
Introduction to Panniculectomy
Panniculectomy is a surgical procedure designed to remove excess skin and fat, typically from the abdomen, often after significant weight loss. This procedure aims to improve the patient’s physical appearance and potentially alleviate discomfort associated with the excess tissue. It’s a common aesthetic surgery, but it’s crucial to understand the procedure, patient profile, and potential risks and benefits before undergoing it.The procedure involves carefully removing the excess skin and fat, typically with incisions strategically placed to minimize scarring.
Different techniques are used depending on the extent of the excess tissue and the patient’s individual needs. The goal is not just removal, but also to achieve a smooth, contoured appearance.
Types of Panniculectomy Procedures
Various approaches to panniculectomy exist, each tailored to specific patient needs. Some procedures focus on minimal scarring, while others address more extensive areas of excess tissue. These variations impact the recovery time and the long-term outcome.
- Standard Panniculectomy: This involves the removal of the excess skin and fat from the abdomen, typically along the lower abdominal area. The incision lines are often carefully placed to minimize visible scarring.
- Modified Panniculectomy: This technique may be used for patients with less extensive excess skin, potentially reducing the length of the incision compared to a standard procedure. It focuses on targeted removal of the pannus, while preserving surrounding healthy tissue.
- Combined Procedures: In some cases, a panniculectomy may be combined with other procedures, such as liposuction or a tummy tuck, to achieve a more comprehensive aesthetic result. This is often done for individuals with significant excess tissue or who desire a more substantial alteration of their physique.
Patient Profile for Panniculectomy
The typical patient seeking a panniculectomy is someone who has experienced significant weight loss and is left with excess skin and fat, often leading to discomfort and body image issues. The procedure is not intended for individuals looking for weight loss or to treat underlying medical conditions. Patients are typically in good overall health, with no significant medical conditions that would pose a heightened risk during or after surgery.
A detailed medical history and physical examination are essential to ensure the procedure is appropriate for the individual.
Potential Benefits and Risks of Panniculectomy
| Benefit | Risk |
|---|---|
| Improved body image and self-esteem | Infection |
| Reduced discomfort from excess skin and fat | Bleeding |
| Improved mobility and physical function (in some cases) | Scarring |
| Enhanced physical appearance | Nerve damage (rare) |
| Improved comfort in clothing and daily activities | Blood clots |
| Reduced risk of skin irritation and rubbing | Swelling and bruising |
| Improved confidence and well-being | Delayed healing |
Aetna Coverage Policies

Aetna, like many insurance providers, has specific guidelines for covering cosmetic procedures. Understanding these policies is crucial for patients considering procedures like panniculectomy to ensure they’re aware of potential out-of-pocket costs and the necessity of pre-authorization. These guidelines help maintain the balance between patient needs and the insurance company’s financial responsibility.Aetna’s approach to cosmetic procedures generally follows a medical necessity framework.
This means that the procedure must be deemed medically necessary, rather than simply for aesthetic improvement. The medical necessity assessment typically considers factors like the patient’s health status, the severity of the condition being addressed, and the potential benefits of the procedure relative to the risks involved. This approach helps to ensure that resources are used effectively and that procedures are undertaken only when appropriate.
Aetna’s Policy on Panniculectomy
Aetna’s coverage for panniculectomy, a surgical procedure to remove excess skin and fat from the abdomen, is contingent on the presence of a demonstrable medical condition. While aesthetic improvement is a consideration, the primary justification for coverage must be the treatment of a medical condition. This may include, but is not limited to, complications stemming from excess skin and fat, such as skin breakdown, infections, or pain.
The medical necessity must be clearly articulated in the documentation submitted for pre-authorization.
Factors Aetna Considers in Coverage Requests
Aetna evaluates panniculectomy coverage requests based on several factors. These factors include the patient’s medical history, the extent of the excess skin and fat, the presence of any associated medical complications, and the potential risks and benefits of the procedure. The procedure’s appropriateness for the patient’s specific condition and anticipated outcomes is also a key consideration. For example, a patient with severe skin breakdown or chronic pain related to excess abdominal tissue is more likely to have a panniculectomy deemed medically necessary compared to a patient with only cosmetic concerns.
Documents Typically Required for Aetna Coverage
Aetna requires comprehensive documentation to support pre-authorization requests for panniculectomy. A well-structured pre-authorization request significantly increases the likelihood of approval. A structured approach ensures all pertinent information is included.
While Aetna’s coverage of panniculectomy procedures varies, consideration of patient demographics and specific medical needs is crucial. This evaluation often overlaps with factors like family entertainment preferences, such as frequent visits to establishments like family video and marco’s pizza , which can influence overall healthcare expenditure and potentially affect the insurance coverage decision for panniculectomy procedures.
- Complete medical records: This includes detailed patient history, physical examinations, diagnostic tests, and any previous treatments related to the condition.
- Detailed justification for medical necessity: This should clearly articulate how the panniculectomy addresses a medical condition, not just an aesthetic concern. Specific details about the patient’s symptoms, the impact on their quality of life, and the potential benefits of the procedure must be clearly stated.
- Physician’s statement: A detailed letter from the surgeon outlining the medical rationale for the procedure, the patient’s specific medical condition, and the anticipated outcomes. The physician should also clearly document the expected risks and benefits and why this particular procedure is the most appropriate treatment.
- Imaging studies: Relevant imaging studies, such as X-rays, CT scans, or MRIs, may be necessary to demonstrate the extent and nature of the condition requiring treatment.
- Patient’s consent form: A signed consent form from the patient authorizing the procedure.
Pre-Procedure Considerations
A successful panniculectomy hinges on thorough pre-operative evaluations. These assessments ensure patient safety, optimize surgical outcomes, and minimize potential complications. Careful consideration of medical history, physical examination findings, and patient counseling are critical components of this process.Pre-operative evaluations encompass a multifaceted approach aimed at identifying any potential risks and ensuring the patient is well-prepared for the procedure. This proactive approach minimizes the chances of unexpected complications during and after surgery.
Proper evaluation helps tailor the surgical plan and anesthesia approach to individual patient needs, resulting in a more personalized and successful procedure.
Pre-Operative Evaluations and Assessments
Pre-operative evaluations serve as a crucial foundation for successful panniculectomy. These evaluations provide a comprehensive understanding of the patient’s health status, allowing the surgical team to assess risks and plan the best course of action. This detailed assessment process involves multiple steps, including a comprehensive medical history review, physical examination, and patient counseling.
Medical History Review Process
A thorough review of the patient’s medical history is paramount. This review identifies any pre-existing conditions, allergies, medications, and past surgical experiences that might impact the procedure or increase the risk of complications. Detailed documentation of all relevant information is essential for informed decision-making. This includes past surgeries, hospitalizations, chronic conditions, and current medications. Reviewing previous surgical records and medical reports from other healthcare providers is critical for a comprehensive understanding of the patient’s health history.
The information gathered helps in identifying potential complications, planning appropriate anesthesia protocols, and tailoring the surgical approach.
Role of Physical Examinations
Physical examinations are essential for assessing the patient’s overall health and identifying any potential issues. These examinations evaluate vital signs, body composition, and other relevant physical characteristics. The physical examination helps assess the patient’s general health, identifying any conditions that could impact the surgical procedure. It also helps determine the patient’s overall physical condition, including body mass index (BMI), mobility, and other factors.
Importance of Pre-Operative Counseling
Pre-operative counseling is crucial for preparing the patient psychologically and physically for the surgery. This counseling process involves explaining the procedure, potential risks and benefits, recovery expectations, and post-operative care instructions. Open communication fosters trust and empowers the patient to make informed decisions. Detailed explanations about the surgical procedure, potential complications, and the recovery process are essential components of pre-operative counseling.
This ensures the patient understands the procedure, its potential outcomes, and their responsibilities in the recovery process. Realistic expectations about the procedure’s effectiveness and post-operative recovery are crucial.
Examples of Pre-Operative Patient Questionnaires
Pre-operative patient questionnaires provide a structured way to gather essential information. These questionnaires cover various aspects of the patient’s health, lifestyle, and medical history. The information collected helps assess risk factors, plan appropriate interventions, and tailor the surgical approach. Example questions might include:
- Detailed medical history, including past surgeries, hospitalizations, and chronic conditions.
- Current medications, including prescription drugs, over-the-counter medications, and herbal supplements.
- Allergies to medications, latex, or other substances.
- Current or recent illnesses or infections.
- Family history of medical conditions, including cardiovascular disease, blood clots, and bleeding disorders.
- Lifestyle factors, such as smoking, alcohol consumption, and diet.
- Previous experiences with anesthesia or similar procedures.
- Expectations and concerns regarding the procedure and recovery.
These questionnaires are designed to collect comprehensive data to ensure a safe and effective surgical procedure. They help in identifying any potential issues or concerns that might affect the patient’s health status before surgery.
Insurance Claim Process
Navigating the insurance claim process for a panniculectomy can be complex. Understanding the steps, required documentation, and potential appeals pathways is crucial for a smooth and successful outcome. This section details the process specifically for Aetna insurance.
Submitting a Panniculectomy Claim to Aetna
The claim submission process involves several key steps. Proper documentation at each stage is vital for a successful claim. Aetna’s claim procedures typically require pre-authorization for surgical procedures.
Pre-authorization
Prior authorization is a critical step in the claim process. Aetna requires pre-authorization to ensure the procedure aligns with their coverage guidelines. Aetna’s pre-authorization requirements include detailed medical documentation supporting the necessity of the panniculectomy. This often includes patient history, physical examinations, and supporting medical reports justifying the procedure.
- Obtain a pre-authorization request form from Aetna. This form Artikels the specific information required by Aetna for pre-authorization.
- Complete the form accurately and thoroughly. Inaccurate or incomplete information may delay or deny pre-authorization. Include detailed patient medical records and any supporting documentation related to the medical necessity of the procedure.
- Submit the pre-authorization request to Aetna via their designated channels. These channels can include online portals, fax, or mail. Ensure the form is submitted with all required supporting documents.
Claim Submission
After pre-authorization, you will need to submit the claim itself. This process often involves submitting the necessary medical bills and supporting documentation.
- Gather all relevant medical records, including the pre-authorization approval letter. This comprehensive collection includes the patient’s medical history, surgical reports, and any pre- and post-operative physician notes.
- Submit the claim electronically via Aetna’s online portal or using the method specified by Aetna. Confirm the claim is properly submitted by checking for a confirmation receipt. This receipt should acknowledge the claim’s acceptance and provide a claim ID for tracking purposes.
- Ensure all required information, such as the physician’s information, procedure codes, and dates, is accurate. Inaccurate information may lead to claim delays or rejections.
Appealing a Denied Claim
If your claim is denied, Aetna has an appeals process. A timely and well-documented appeal is essential for reconsideration.
- Review the denial letter carefully. Understand the specific reasons for denial. This involves noting the precise reasons cited for the claim’s rejection, and any supporting documentation that Aetna has provided.
- Contact Aetna’s customer service department or dedicated appeals team. Discuss the denial and any supporting evidence that you believe was overlooked. Explain the reasons for the procedure’s necessity and any relevant information that was not considered during the initial claim review.
- Provide supporting documentation to support your appeal. This includes additional medical records, physician statements, and any other evidence that strengthens the case for the procedure’s medical necessity. Highlight any new information that may not have been available during the initial claim process.
Common Reasons for Claim Denials
Aetna may deny a panniculectomy claim for various reasons. Understanding these reasons can help prevent future denials.
| Reason | Explanation |
|---|---|
| Lack of medical necessity | Aetna may deny the claim if they deem the procedure not medically necessary based on the provided documentation. |
| Inadequate pre-authorization | Failure to obtain pre-authorization or incomplete pre-authorization request form. |
| Incorrect procedure codes | Incorrect or missing procedure codes used in the claim submission. |
| Missing documentation | Absence of crucial supporting medical documents, such as physician’s notes or pre-operative evaluations. |
| Patient’s pre-existing conditions | In some cases, pre-existing conditions may influence the claim’s approval, and Aetna may need further documentation to clarify their impact on the procedure. |
Alternatives and Comparisons
Choosing the right body contouring procedure requires careful consideration of various factors, including individual needs, desired outcomes, and potential risks. Understanding the alternatives to panniculectomy, and their respective advantages and disadvantages, is crucial for informed decision-making. This comparison helps patients evaluate the suitability of different options based on their unique circumstances.
Comparison to Liposuction
Liposuction, a popular procedure for reducing localized fat deposits, differs significantly from panniculectomy in its approach and target areas. Liposuction primarily removes fat, while panniculectomy addresses excess skin and tissue. Patients with significant skin redundancy may not achieve optimal results with liposuction alone. This is because liposuction does not address the underlying skin laxity often associated with significant weight loss or aging.
The long-term outcomes of liposuction generally include a reduction in fat in the targeted areas. However, skin laxity can still remain, potentially leading to loose or uneven skin appearance over time.
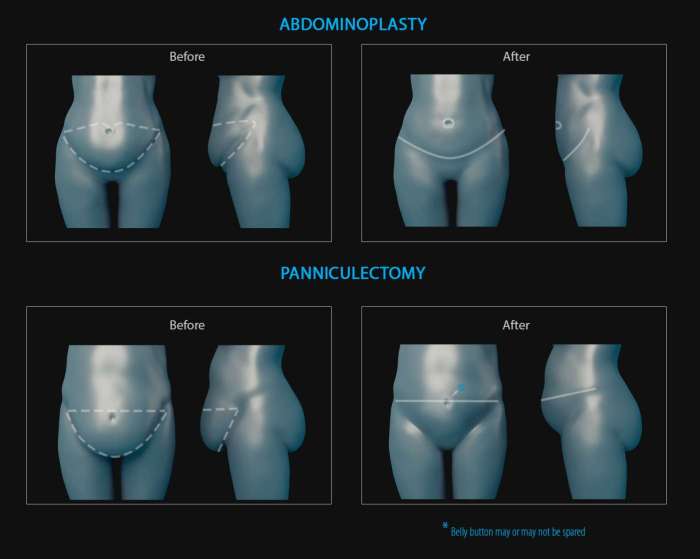
Comparison to Abdominoplasty (Tummy Tuck)
Abdominoplasty, commonly known as a tummy tuck, addresses abdominal skin laxity and excess fat, similarly to panniculectomy. However, the scope of the procedure differs. A panniculectomy focuses solely on removing the excess skin and fat hanging from the abdomen, while abdominoplasty also tightens the underlying abdominal muscles, repositioning the remaining skin. The long-term outcomes of abdominoplasty often include improved abdominal contour and reduced skin laxity, but it carries a higher degree of invasiveness than panniculectomy.
Potential complications include, but are not limited to, infection, bleeding, and scarring.
Comparison to Laser-Assisted Liposuction (LAL), Panniculectomy covered by insurance aetna
Laser-assisted liposuction (LAL) combines the principles of liposuction with laser energy. The laser helps to refine the contour and reduce inflammation, but it does not address the excess skin associated with panniculectomy. Therefore, LAL is less effective for patients with significant skin laxity and more appropriate for individuals with localized fat deposits and minimal skin redundancy. Potential long-term outcomes include improved contouring of treated areas, reduced inflammation, and potentially enhanced results when combined with other procedures.
However, the effectiveness in treating excess skin is limited compared to a panniculectomy.
Comparison to Body Wraps and Other Non-Surgical Options
Body wraps and other non-surgical options aim to reduce the appearance of excess fat and skin through temporary techniques. These methods do not address the underlying causes of skin laxity or fat accumulation. The long-term outcomes of body wraps are generally limited to temporary improvements in appearance. These methods may offer minimal long-term impact on body contour and may not address the structural issues underlying excess skin.
Significant weight loss or skin laxity often necessitates surgical intervention for lasting results.
Summary Table
| Procedure | Pros | Cons |
|---|---|---|
| Panniculectomy | Addresses significant skin redundancy; improves abdominal contour; effective for patients with extensive excess skin. | Higher invasiveness; longer recovery time; potential for scarring; risk of complications. |
| Liposuction | Relatively less invasive; shorter recovery time; suitable for localized fat deposits. | Does not address excess skin; may not yield optimal results for patients with significant skin laxity. |
| Abdominoplasty | Tightens abdominal muscles; improves overall abdominal contour; more comprehensive approach. | Higher invasiveness; longer recovery time; greater potential for complications than panniculectomy. |
| Laser-Assisted Liposuction | Can enhance contouring results; potentially reduces inflammation. | Less effective for addressing significant skin laxity; not a substitute for panniculectomy for extensive skin redundancy. |
| Body Wraps/Non-Surgical Options | Non-invasive; generally low cost. | Limited long-term effectiveness; does not address underlying causes of skin laxity or fat accumulation. |
Potential Complications and Recovery
Panniculectomy, while often a successful procedure for improving body contour, carries potential risks and requires a meticulous recovery process. Understanding these aspects is crucial for patients to make informed decisions and ensure a smooth return to health. Proper post-operative care, adherence to physician instructions, and proactive management of potential complications are key to a positive outcome.
While Aetna’s coverage for panniculectomy procedures varies based on individual circumstances, a crucial aspect of patient well-being post-surgery is often overlooked. Consideration for appropriate post-operative activities, such as visiting nail salons in Janesville WI nail salons in janesville wi , can contribute to improved patient comfort and recovery. Ultimately, comprehensive evaluation of all factors is essential when determining insurance coverage for panniculectomy procedures under Aetna’s guidelines.
Potential Complications
Post-operative complications, while relatively infrequent, can occur after panniculectomy. These complications range from minor issues to more serious concerns. A thorough understanding of potential problems allows for proactive measures to mitigate their impact.
- Infection: Infection at the incision site is a possible complication. Antibiotics may be prescribed to prevent or treat infections. Prompt reporting of any signs of infection, such as increased pain, swelling, redness, or pus, is essential. Proper wound care, including meticulous hygiene and dressing changes, is crucial in preventing infection.
- Hematoma: Blood clots, or hematomas, can form at the surgical site. This can lead to swelling, pain, and potentially require drainage. Proper compression garments and elevation of the affected area are often recommended to reduce the risk of hematomas.
- Seromas: Fluid buildup, known as seromas, can occur under the skin. This can cause swelling and discomfort, and sometimes requires aspiration to drain the fluid. Early intervention by the healthcare provider can prevent significant complications.
- Nerve Damage: Although rare, nerve damage is a possible complication. This can result in numbness, tingling, or altered sensation in the treated area. This typically resolves over time, but persistent issues may require further evaluation.
- Deep Vein Thrombosis (DVT): Blood clots in the deep veins of the leg are possible, and DVT can lead to significant complications. Early mobility, compression stockings, and anticoagulant medications are often prescribed to minimize the risk of DVT.
- Skin Discoloration/Scarring: Changes in skin tone or the formation of noticeable scars are potential outcomes. The extent of scarring varies depending on the individual and the surgical technique used. Scarring often fades over time, but in some cases, further treatment might be considered.
Recovery Timeframes
The recovery period following panniculectomy is typically several weeks. Individual recovery times can vary based on factors such as the patient’s overall health, the extent of the surgery, and adherence to post-operative care instructions.
A typical recovery timeframe can range from 4-8 weeks, with complete healing taking several months.
Post-Operative Care
Adherence to post-operative care instructions is crucial for a successful recovery. This includes diligently following the prescribed pain management regimen, maintaining proper wound care, and avoiding strenuous activities.
- Pain Management: Pain medication is typically prescribed to manage post-operative discomfort. It is crucial to take the prescribed medications as directed to manage pain effectively.
- Wound Care: Maintaining the cleanliness and integrity of the surgical wound is vital. Patients should follow the specific instructions from their surgeon regarding dressing changes and wound care.
- Activity Restrictions: Avoid strenuous physical activity for the first few weeks to allow the surgical site to heal. This includes lifting heavy objects, prolonged standing, and intense exercise.
- Compression Garments: Compression garments or bandages may be recommended to reduce swelling and support the healing process. These are often worn for several weeks to aid in the healing process.
- Nutrition and Hydration: A healthy diet and adequate hydration support the body’s healing process. This includes consuming nutritious foods and maintaining proper fluid intake.
Follow-up Appointments
Regular follow-up appointments are essential to monitor the healing process and address any concerns or complications. These appointments allow the surgeon to assess the wound’s progress, address any issues, and provide ongoing support.
Potential Complications Summary
| Potential Complication | Likelihood | Severity |
|---|---|---|
| Infection | Moderate | Potentially Significant |
| Hematoma | Moderate | Moderate |
| Seromas | Moderate | Moderate |
| Nerve Damage | Low | Potentially Significant |
| DVT | Low | Significant |
| Skin Discoloration/Scarring | Moderate | Minor to Moderate |
Provider and Facility Considerations
Choosing the right healthcare provider and facility is crucial for a successful panniculectomy. This involves careful consideration of qualifications, experience, and facility capabilities. A qualified surgeon and a well-equipped facility contribute significantly to positive outcomes and a smoother recovery process. Factors like board certifications, experience levels, and the facility’s post-operative care protocols are key to making informed decisions.
Qualified Healthcare Providers
Panniculectomy requires specialized surgical expertise. Plastic surgeons, general surgeons, and some other surgical specialists are often qualified to perform this procedure. However, experience level significantly impacts the outcome. Surgeons with extensive experience in panniculectomy procedures are more likely to provide superior surgical technique and patient care.
Facility Selection
Selecting a qualified facility is just as important as choosing a qualified surgeon. A well-equipped facility with advanced surgical capabilities, experienced nursing staff, and a dedicated post-operative care unit is essential for a safe and efficient recovery. This includes proper facilities for wound care, pain management, and potential complications.
Board Certifications and Experience Levels
Board certification in plastic surgery or general surgery demonstrates a surgeon’s commitment to maintaining a high standard of practice. This certification signifies that the surgeon has met specific training and experience requirements. Moreover, the surgeon’s experience with panniculectomy procedures directly impacts the outcome. A surgeon with a proven track record of successful panniculectomy procedures demonstrates a higher degree of proficiency and reduces potential complications.
Experience translates to better surgical techniques and a greater understanding of post-operative care.
Comparing Facilities and Practices
Different facilities may have varying practices and protocols. Researching different facilities and their surgical protocols, such as pain management techniques and post-operative care, is important. Reviewing patient testimonials and outcomes can offer valuable insights into a facility’s success rate and approach. Comparing the experience and success rates of different surgeons and facilities can help potential patients make an informed decision.
For example, a facility with a specialized post-operative care unit and a dedicated wound care team might be a better option than a facility with less robust post-operative support.
Questions to Ask a Potential Surgeon
Thorough preparation involves asking the potential surgeon key questions about their experience and approach to panniculectomy. Examples of such questions include:
- How many panniculectomies have you performed?
- What is your approach to managing post-operative pain?
- What is your facility’s protocol for wound care and infection prevention?
- What are the potential risks and complications of the procedure?
- What is your experience with specific complications and how do you handle them?
- What is the estimated recovery time and expected outcome?
These questions help patients understand the surgeon’s expertise, approach to the procedure, and the facility’s post-operative care protocol. These factors contribute to a successful and safe procedure.
Illustrative Case Studies (Hypothetical)
Understanding how Aetna’s coverage policies apply to panniculectomy procedures requires examining real-world scenarios. These hypothetical case studies highlight different patient profiles, medical histories, and potential outcomes, demonstrating the complexities involved in coverage decisions. These examples, while hypothetical, reflect common factors that influence the approval process.
Case Study 1: The Healthy Patient with Strong Motivation
This patient, a 45-year-old female with no significant medical history, is motivated to undergo panniculectomy for cosmetic reasons. She has a strong desire to improve her self-image and quality of life, but is otherwise healthy.
- Pre-operative Considerations: The patient’s health status is excellent, presenting minimal pre-operative risks. Aetna’s coverage criteria, likely focused on the medical necessity and appropriateness of the procedure, will be crucial in this case.
- Aetna Coverage Application: Given the patient’s healthy status and strong motivation, the procedure is likely to be considered medically necessary for cosmetic reasons, provided it meets the criteria Artikeld by Aetna. Factors like the extent of excess skin and the patient’s overall well-being are likely to influence the decision.
- Decision-Making Process: Aetna’s decision-making process may involve a review of the patient’s medical records, justification for the procedure, and comparison to established criteria for coverage of cosmetic procedures. The outcome hinges on the provider’s documentation and the patient’s clear articulation of their needs.
- Post-operative Experience: A healthy recovery is expected, with minimal complications. The patient will likely experience a period of discomfort and swelling, but full recovery is anticipated.
Case Study 2: The Patient with Underlying Health Conditions
This 60-year-old male patient has a history of hypertension and type 2 diabetes. He seeks panniculectomy for both cosmetic and functional reasons, as the excess skin impacts mobility.
- Pre-operative Considerations: The patient’s underlying health conditions increase the pre-operative risks. A comprehensive medical evaluation is essential to assess the patient’s overall health and suitability for the procedure. Thorough pre-operative evaluations, including blood tests and assessments of cardiac and pulmonary function, will be crucial.
- Aetna Coverage Application: Aetna’s coverage policies will likely prioritize the medical necessity of the procedure, particularly considering the patient’s existing conditions. The procedure’s impact on his mobility and well-being will be considered, potentially influencing the decision regarding medical necessity.
- Decision-Making Process: Aetna will scrutinize the documentation to ensure that the procedure is necessary to address functional issues. The severity of his conditions and the potential risks associated with the surgery will significantly influence the coverage decision.
- Post-operative Experience: The patient’s recovery might be slower and more complicated due to the presence of pre-existing conditions. Careful management of blood sugar levels and blood pressure will be critical during the recovery period.
Case Study 3: The Patient with Complicated Procedure
A 55-year-old female patient requires a more extensive panniculectomy due to the significant amount of excess skin and associated complications.
- Pre-operative Considerations: The patient’s need for a more complex procedure increases the pre-operative risks, requiring a more thorough evaluation of the patient’s overall health status and the potential risks associated with the procedure. A comprehensive surgical plan, factoring in the extensive nature of the procedure, is necessary.
- Aetna Coverage Application: Aetna’s coverage policies will likely scrutinize the complexity of the procedure and its necessity, considering the potential complications and the patient’s overall health. The provider’s documentation justifying the complexity and necessity will be crucial.
- Decision-Making Process: Aetna’s review will encompass the complexity of the procedure, the patient’s health status, and the potential risks. A detailed explanation from the surgical team regarding the necessity and anticipated outcomes will be vital in the decision-making process.
- Post-operative Experience: Recovery from a complex panniculectomy can be more challenging and potentially prolonged. The patient may experience a higher degree of discomfort and complications. Close monitoring and management of potential complications will be paramount during the recovery period.
Final Review
In conclusion, understanding panniculectomy coverage under Aetna insurance involves careful consideration of the procedure itself, Aetna’s policies, and pre-operative and post-operative factors. This comprehensive guide provides valuable insights to help you navigate the process. By understanding the procedure, Aetna’s requirements, and potential complications, you can make well-informed decisions about your health journey.
User Queries: Panniculectomy Covered By Insurance Aetna
What are the typical recovery timeframes for panniculectomy?
Recovery times vary, but most patients experience a gradual return to normal activities within several weeks. Post-operative care, including follow-up appointments, is crucial for optimal healing.
What are some common reasons for a claim denial regarding panniculectomy?
Aetna may deny coverage if the procedure isn’t deemed medically necessary, if the patient doesn’t meet specific criteria, or if supporting documentation isn’t complete. It’s crucial to understand Aetna’s specific requirements to avoid potential denials.
Are there alternative body contouring procedures besides panniculectomy?
Yes, other options like liposuction, abdominoplasty, and skin tightening techniques exist. Each procedure has its own advantages and disadvantages, and a consultation with a qualified healthcare provider is essential for evaluating suitable alternatives.
What documents are typically required for Aetna coverage of a panniculectomy?
The required documentation often includes pre-operative evaluations, medical records, and a detailed explanation of the procedure’s medical necessity. Consulting Aetna’s website or contacting their customer service can provide a complete list of needed paperwork.
